Abstract
Background
Watchful waiting (WW) is a widely accepted approach for asymptomatic patients with follicular lymphoma (FL) as studies have shown no survival differences between WW and immediate chemotherapy in the pre-Rituximab (R) era. The risk of WW is progressive disease resulting in significant organ dysfunction or transformation to aggressive histology lymphoma, potentially impacting quality of life and success of subsequent therapy relative to that achieved with immediate R-chemotherapy. These risks and adverse sequelae are not clearly reported in the WW literature. The objectives of our study were to evaluate the frequency of such adverse events of WW, and determine if these events impact long-term time to progression (TTP) or overall survival (OS). Additionally, we compared outcomes of R-chemotherapy for patients who were initially managed by WW with a separate dataset of patients who underwent immediate R-chemotherapy for symptomatic or high tumor burden.
Methods
Records of newly diagnosed patients aged 18-70 years with FL grade 1-3a from Calgary (1994-2011) and Edmonton (2001-2010) were retrospectively reviewed to identify those managed with an initial WW strategy (>90 days from diagnosis to first active treatment), and evaluate long-term outcomes. Baseline demographics including age, gender, stage, bulk, and FL international prognostic index (FLIPI) were recorded. Patients treated with immediate R-chemotherapy (with or without maintenance) during the same time periods from both centres were identified as a comparator group to those WW patients who were treated with R-chemotherapy at the time of progression. Study endpoints included: initial time to progression requiring therapy (TTPRT), transformation, significant organ dysfunction, TTP following first R-chemotherapy, and OS. Significant organ dysfunction categories were based on GELF high tumor burden criteria and severity of extranodal involvement decided by author consensus. Survival analysis was performed using the Kaplan-Meier method and logrank test, and p values <0.05 were considered significant.
Results & Discussion
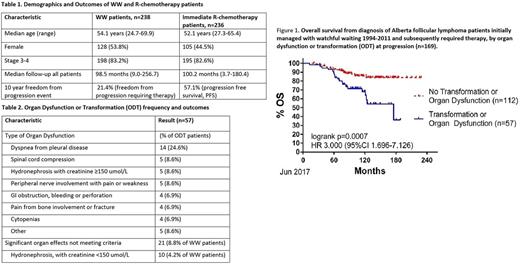
Out of a consecutively diagnosed series of 824 follicular lymphoma patients, 238 (28.5%) were initially managed with WW. Baseline demographics and outcomes are outlined in Table 1. Median follow-up (mFU) was 98.5 (9.0-256.7) months (mo) for all 238 patients, during which 169 patients (71.0%) progressed and required therapy. The median TTPRT was 46.8 mo, and by multivariate analysis was only associated with > 5 nodal sites at diagnosis (30.9 vs 55.8mo, HR 1.66 (95%CI 1.14-2.43), p=.009).
Among those who progressed, 57 (23.9% of total and 33.7% progressors) developed the composite outcome of organ dysfunction or transformation (ODT) at a median of 29.9mo (3.3-114.8). There were no predictors of ODT by univariate or multivariate analyses. At the time of ODT, 56 patients received treatment with chemotherapy; R-CHOP (n=25, 43.9%), R-CVP (n=15, 26.3%), bendamustine with rituximab or obinutuzumab (n=6, 10.5%), or other regimens including non-rituximab containing chemotherapy (n=10, 17.5%). Of those who progressed requiring therapy, 10 year OS was significantly worse in those with transformation (65.4 vs 83.2%, HR 2.88, p=0.002), organ dysfunction (72.1 vs 82.6%, HR 2.04, p=0.035) and ODT (67.9 vs 85.7%, HR 3.00, p=0.001, see figure 1).
Comparing the 133 WW patients who received R-chemotherapy as first treatment to a separate cohort of 236 patients who received immediate R-chemotherapy, we found no difference in TTP measured from the time of treatment initiation (p=0.51), and no difference in 10-year OS measured from time of diagnosis (p=0.612). However, 10-year OS from the time of R-chemotherapy was inferior for patients who had previously undergone a period of WW (74.4% vs. 84.0%, p=0.022). Additionally, the transformation rate during long term follow up for patients managed with initial WW who progressed requiring treatment was much higher than those who received immediate R-chemotherapy (21.1% vs. 8.1%, p=0.0003).
In conclusion, our study demonstrated benefits of WW including a 29% chance of not requiring treatment at 98mo mFU. However, the risks of WW including a 24% rate of ODT and subsequent inferior OS need to be better recognized and explained to patients who consent to the WW approach. This consent process should be repeated for patients who are asymptomatic but clearly progressing during WW.
Peters: Lundbeck: Honoraria; Roche: Honoraria; Gilead: Honoraria; Abbvie: Honoraria; Janssen: Honoraria. Stewart: Gilead: Honoraria; Janssen: Honoraria; Servier: Honoraria; Amgen: Honoraria; Roche: Honoraria; Abbvie: Honoraria; Seattle Genetics: Honoraria; BMS: Honoraria; Merck: Honoraria; Lundbeck: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal